With an increase in value-based programs driving demand for enhanced data sharing between health plan payers, providers, and a growing list of 3rd party intermediaries charged with facilitating accessibility and care management services, the ability to efficiently share the right data at the right time to the right recipient is rapidly becoming table stakes for operating in today’s competitive healthcare environment. In fact, multiple regulations, policy directives, and technical specifications like the Interoperability and Patient Access final rule, ONC’s Cures Act Final Rule, and Fast Healthcare Interoperability Resources (FHIR) are making specific demands upon healthcare stakeholders to provide meaningful interoperability more urgent and important than ever.
In our 3rd Focus Area Roundtable on Interoperability that took place last week, fourteen experienced healthcare professionals representing a cross-section of healthcare stakeholders shared ideas for implementing practical, short-term, interoperable data exchange among their representative organizations. This post shares some of the discussion facilitated by Surescripts and presents a checklist for delivering meaningful interoperability over the next 12 months.
Healthcare Interoperability Challenges Shared in Earlier Roundtables
HCEG’s Executive Director Ferris Taylor kicked off the discussion and helped set for the roundtable by sharing poll results and some highlights from earlier roundtables on interoperability. He acknowledged the importance of privacy, security, and cybercrime concerns in the healthcare marketplace, particularly on the provider side and noted that interoperability-related privacy and security would not be addressed in the roundtable discussion.
RELATED: Discussing Barriers to Healthcare Interoperability, Use-Cases, and More – Part 1
Approaches to Establishing Meaningful Interoperability Pathways
Tim Capstick and Ashley Clark, two Surescripts executives who interact with national, regional, and small health plans on a regular basis, shared that there are a lot of different strategies given payer might deploy to gain meaningful use across their interoperability initiatives. Some payers are working directly with vendors of electronic health record (EHR) systems but, due to the number of EHR technology vendor solutions that exist in the marketplace, they’re often only able to realistically integrate with a limited number of endpoints – typically EHR systems but also health information exchanges (HIE) and other sources of clinical, financial, and administrative data. Tim noted the existence of a potential 700 different EHR entities any single health plan would have to find some way to connect with to achieve near-complete interoperability.
This large number of integration pathways and endpoints are a big part of the reason why Surescripts, which already connects with 98% of the EMRs, and others like Carequality and CommonWell Health Alliance – two organizations focused on advancing healthcare interoperability – are striving to provide healthcare stakeholders with the ability to connect across the healthcare ecosystem and work more efficiently.
Pathways for Connecting Endpoints Across the Healthcare Ecosystem

See A Faxless Future: Dare We Dream?
Using health information exchanges (HIE) that many, but not all, states have stood up over the past decade was noted as another pathway to connectivity. While pros and cons to using HIE’s were not discussed, use cases incorporating HIE’s were noted as a potentially viable approach for payers and providers in states and regions with well-developed exchanges.
Engaging with Health Plans to Achieve Meaningful Interoperability: An Ongoing Challenge
The executive director of an organization working to provide a national-level, consensus-built, common interoperability framework to enable exchange between and among healthcare data sharing networks offered that his organization is doing a lot with provider-to-provider exchange that makes up the bulk of stakeholder organization data exchanges. He noted a level of difficulty getting payers involved with defining use cases supporting connectivity and data exchange.
He also confirmed Tim’s comment about some large payers working directly with the EHR vendors and went on to share that some straw use case proposals developed between a national plan and leading EHR vendor are being used by his organization to get other payers involved as a starting point for obtaining payer feedback.
Use Cases – Defining the Purpose of Payer-Provider Data Exchange is Critical
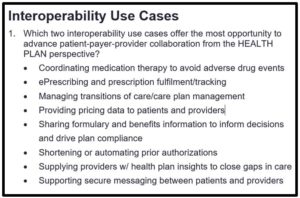
Organizations are not comfortable with over-sharing data so it’s important to understand, at the most granular level, what the recipient is trying to accomplish in order to make a determination of what data to release. Breaking out data exchange use cases into clearly-defined sub-categories so provider organizations are comfortable sharing data for well-defined usage scenarios is necessary.
Limitations Due to Geographic and Technology Vendor Products
Other barriers to address for increased interoperability between healthcare stakeholders is that connectivity and exchange of data are typically limited to specific network membership and often restricted to specific geographic and/or technology vendor product lines or capabilities. The value of partnering to avoid the need to develop one-off, health data sharing, legal agreements between a multitude of individual data-sharing partners was noted as a means of accelerating the delivery of less costly data exchanges.
Help Define Payer-Provider Data Exchange Policy – Join a Carequality Workgroup
Healthcare payers and providers interested in further helping define payer-provider data exchange and communications may want to investigate a new Interoperability Framework workgroup that Carequality is starting at the beginning of the new year.
The goal of the group will be to create policies that will allow payers to easily access patient information from all Carequality Connected providers without needing out-of-band coordination or agreements, etc., with policies that allow those providers to “trust” queries from payers; such as the issue discussed in the roundtable where payment and health care operations use cases under HIPAA are too broadly defined and providers are reluctant to share data. Learn more about Carequality and this new workgroup here.
RELATED: Importance of Establishing & Maintaining Trust to Overcome Barriers to Practical Interoperability
Electronic Health Record Systems as a Mechanism for Payer-Provider Communication
A regional medical officer of a national health plan operating in multiple states shared the importance of meaningful interoperability with EHR’s as a means to access clinical data and communicate with clinicians on a timely basis for the purpose of closing gaps of care for HEDIS, STARS, and other quality measures – measures typically related to risk-adjustment and population health
Like others on the roundtable, she noted challenges in obtaining direct access to EHR’s from network providers, medical groups, and IPA’s. While some organizations allow access, many others do not – preferring to supply charts and access to needed data via SFTP, faxes, or through a 3rd party vendor.
To mitigate the lack of access to EHR data and provide a channel for messaging with clinicians and other front-line staff, she noted her health plan participates in a statewide Health Information Exchange network. Challenges exist in participating in some HIE’s because some states – like California and other large states have multiple HIE networks both at the state and regional areas as well.
Dearth of 3rd Party EHR Data Access Tools Compliant with Industry Standards
The chief information officer of a health plan closely aligned with a provider network echoed the challenges in getting access to data from provider EHRs. He noted the use of a tool from Moxe to connect with provider EHR’s and, also like others, shared many providers’ reluctance to cooperate in providing access to their EHRs.
He noted that obtaining clinical evidence and getting data harmonized to obtain a 360-degree view of a patient to support closing a gap in care can be very difficult. Some plan members may see as many as a dozen different specialists over the course of a year, all using different EHR’s.
The availability of 3rd party EHR data access products compliant with NCQA standards and CMS Interoperability Rules were noted as hurdles.
Importance of Policy to Support Access to Data Maintained by Providers
Surescripts Tim Capstick shared that payers want electronic access to EHR data so they don’t have to perform medical chart chasing, data scraping and continually bothering their network provider practices. Tim noted that it would be great if healthcare stakeholders could more easily access this information through policy changes or some flexibility in implementing some of the existing rules regarding data transparency and interoperability.
Again, the importance of having a clear, formal definition of how specific data is being utilized and reasonable rules dictating access and use of those data was suggested as going a long way in assuring providers comfort with sharing their data.
 Taking the Next Steps Toward Meaningful Interoperability
Taking the Next Steps Toward Meaningful Interoperability
The 3rd Focus Ara Roundtable on Interoperability – like the previous two roundtables facilitated by Surescripts – generated a lot of practical ideas for creating meaningful interoperability. From these discussions, a Checklist for Delivering Meaningful Interoperability in 2022 was developed.
Special thanks to Ashley Clark and Tim Capstick of our sponsor Surescripts for sharing their unique insight throughout the series of roundtables on interoperability. For information on topics presented in this post and to learn more about how to deliver meaningful interoperability at your health plan or provider organization, contact Tim Capstick or Ashley Clark.
To receive additional information on interoperability and other healthcare leader priorities presented on the 2021 HCEG Top 10+ list, subscribe to our newsletter and follow us on Twitter and LinkedIn.
Related Information on Meaningful Interoperability
Building a Foundation of Interoperable Platforms to Facilitate Broad-Based Data Sharing: HIMSS Summary
Policies and Technology for Interoperability and Burden Reduction: CMS Resources Page
Understanding User Needs for Interoperability: Defining Use Cases in eHealth: AHIMA Research
Healthcare System Interoperability – The Key to The Care We All Strive For: HCEG Webinar Recap
Discussing Barriers to Healthcare Interoperability, Use-Cases, and More – Part 1: HCEG Roundtable Recap
Practical Interoperability Part 2: Trust, Workflow, Value-Based Care Models, & More: HCEG Roundtable Recap
Intelligence in Action: Surescripts Resources Page
Interoperability Resources: xtelligent Healthcare Media