
‘Interoperability’ – particularly between health plans and care providers – has been a high priority of healthcare executives for years. It ranks #6 on the 2021 HCEG Top 10+ list and has an impact on almost every area of healthcare. And recent, still evolving mandates regarding data transparency, information blocking, changes to current HIPAA regulations, and interoperability have placed significant challenges upon the health plans, provider organizations, and the technology partners serving the healthcare industry. Forward-thinking stakeholders are not considering mandates as barriers to healthcare interoperability but rather viewing compliance with mandates as opportunities for ensuring the ongoing viability of their healthcare business models.
In our first Focus Area Roundtable on Interoperability held Tuesday, July 20th, and facilitated by our Focus Area Partner Surescripts, leaders from health plans, health systems, and healthcare provider organizations shared their experience, insight, and information in a roundtable fashion on the topic of Interoperability. Surescripts Tim Capstick and Ashley Clark served as industry thought leaders providing their perspective on these interoperability-related topics, in particular from a health plan point of view.
This post presents the first part of a 2-part series sharing highlights of this first roundtable on interoperability. Leaders of health plans, health systems, and provider organizations are encouraged to participate in upcoming Focus Area Roundtables including the 2nd Interoperability roundtable on September 8th, 2021.
Read Part 2 of the recap of this first Focus Area Roundtable on Interoperability here.
Barriers to Healthcare Interoperability Payers & Providers are Encountering
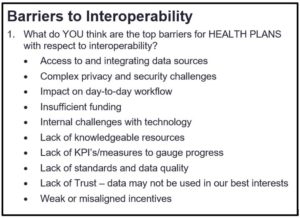
HCEG’s Executive Director Ferris Taylor kicked off the roundtable by asking participants: What are the barriers to healthcare interoperability that health plans and health systems are encountering with respect to the broad topic of interoperability?
Consent Management – One of the Barriers to Healthcare Interoperability
One participant noted that when deploying interoperability solutions, one of the biggest challenges involves consent management for members and patients. Appropriately managing patient data and providing individuals the ability to weigh in on the sharing of their data is both a technical and policy problem. He noted while their organization is addressing consent management largely on their own, he expects the evolution of privacy laws in California and Europe will likely have a national impact across the United States.
Another participant shared that addressing consent management is key to the future of interoperability – not just between members/patients and their health plan and providers but also when providers are sharing information with other health systems/healthcare providers.
Listen here for more on the importance of consent management in advancing interoperability
Other Barriers to Interoperability for Health Plans and Providers
Participants were presented with a list of potential barriers to interoperability and asked to select two barriers from the perspective of a health plan and a provider.
For health plans, Access to and Integrating Data Sources ranked first followed by Complex Privacy and Security Concerns.
For providers, Internal Challenges with Technology and a Lack of Knowledgeable Resources were identified as key barriers to healthcare interoperability.
Impact of Proposed Modifications to HIPAA’s Privacy Rule on Interoperability
Surescripts Ashley Clark shared that data rights are an issue her organization takes very seriously and that they’re currently looking at CMS legislation regarding expanding the definition of treatment under HIPAA and what information can be shared as medical treatment versus non-treatment. Ashley shared that pending regulation changes will likely open up a lot of doors in terms of information that can be shared on things like medication history.
Another participant shared his perspective on barriers to healthcare interoperability for payers and providers by sharing that from his vantage point he’s seeing tremendous reticence on the part of providers to address interoperability and data transparency in any deep way vis-à-vis their health plan partners; with the exception of some relationships forced by the COVID pandemic.
Who Owns Health Plan Member and Provider-Patient Data?
The recent announcement by the Biden Administration to increase penalties on providers who are not making their pricing information available was identified as the first step toward breaking the long-held, culturally ingrained notion that patient care and the information generated from that critical activity belongs to the health system and to the provider community alone. It was noted cultural acceptance – on the part of both payers and providers – that their existing business models are built on a largely zero-sum game is a large barrier that must be overcome in order for practical interoperability to be widely adopted.
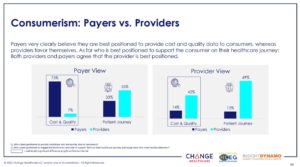
Note: Respondents to the 2020 Industry Pulse Report shared their take on data ownership between payers and providers. See survey results in the graphic on the right.
Listen here to a roundtable participant discuss data ownership among health plans and providers
“Culture eats technology. Culture eats strategy. Culture eats operations. Culture even attempts to eat policy for lunch.” – Roundtable Participant Denny Brennan – Executive Director & Chief Executive Officer of HCEG partner Massachusetts Health Data Consortium
Health Plans as Primary Connection for Patients & Healthcare Consumers
The concept of data hoarding by providers and payers was discussed along with the idea that it’s easier for health plans to surface data than it is for providers to do so. January of 2023 – just over two years away – was noted as a deadline for providers to share almost all of ‘their data’ with health plans. Per the Interoperability and Patient Access final rule (CMS-9115-F), providers will have to send the entire patient medical record to a patient’s current health plan because that health plan is responsible for moving that to the patient’s next health plan.
“I know a lot of regulators and a lot of providers around the country have not yet internalized the idea that the primary connection for the patient is going to be the health plan and that providers are responsible for providing the health plan all the clinical data that’s necessary to maintain that connection. And to inform the patient and make it possible for payer-to-payer connectivity to work.”
RELATED: Key Interoperability, Health Information Technology, and Transparency Policies
How Health Plans Can Best Support Provider Organizations Address Barriers to Healthcare Interoperability
“If I were running a medical group or a community hospital, one of the first things I’d be thinking is:
- How do I sit down with my major payers and figure out what I can upload?
- What am I doing that I don’t have to do that payers can pick up with me?
- How do I cement that partnership by taking over pieces of the business that they insist on taking over that I’m better equipped to do like delivering care to the patient?
I’m the one who’s going to engage the patient. Give me tools, help my staff get trained so that the doctor doesn’t have to talk to the patient about SDOH or the doctor doesn’t have to talk to the patient about their financial exposure.”
Listen here for more on how health plans can help healthcare providers enhance interoperability
Use Cases with Most Potential to Increase Interoperability
Ferris asked participants to share their insight on which use cases might best advance interoperability and improve payer-provider-patient/consumer collaboration.
Increasing Consumer Ownership & Assisting Stakeholders Serve Their Members/Patients
A health plan participant shared that the use cases he sees that have the most impact potential are ones that lead to an increased amount of consumer ownership and activation of the health system to serve the member/patient. He noted that the process of effecting these use cases requires healthcare organizations to face some level of deconstruction. He explained that addressing barriers to interoperability in healthcare means that everyone has to have a relationship with everyone else when it comes to data – and some organizations are uncomfortable with that. So, we have more work to do.
Automating High Friction Activities & Improving Patient Engagement
Another participant shared that his organization separates use cases into two major buckets. One in the realm of automating high friction activities between payers and providers. Frequently occurring activities that can be automated and that are happening in every other industry. And the other in the realm of interventions, population health, or value-based care efforts that actually improve care like patient engagement, chronic disease management, telemedicine, etcetera. For each bucket he emphasized the importance of each use case:
- Being capable of being rolled out on their own and in a stepwise fashion to get to some ideal future state.
- Having deployable value on its own and being able to stand on its own.
As an example of the bucket on the automation side, one of the first things healthcare organizations should address is auto eligibility because something like three-quarters of the calls from providers to their payers is some flavor of eligibility. And, except for a long tale of rare cases, a lot of that is totally automatable.
In a recent Focus Area Roundtable facilitated by HealthSparq, participants discussed how new price transparency mandates will likely help drive opportunities for increased engagement between providers and their patients. Read more about this potential in Payer-Provider Collaboration Critical to Meeting Price Transparency Mandates.
Reshaping Patient Relationships with Providers
Another participant shared that their personal experience is that the patient-provider relationship is typically a transactional relationship – often a negotiation on a chargemaster – and that increased interoperability seems to have the potential at least to change that quite dramatically.
Most Impactful Use Cases Identified by Focus Area Roundtable Participants
After discussing interoperability-related use cases, participants responded to a poll on ‘Which interoperabili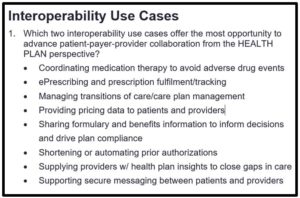
- Shortening or Automating Prior Authorizations
- Providing Pricing Data to Patients & Providers
Electronic Prior Authorizations – Webinar on August 25th at 2:00 PM ET
Automating the processing of prior authorizations via ‘electronic prior authorization’ (ePA) – particularly in settings like the pharmacy where a patient may be waiting – can significantly enhance patient/member engagement by reducing the time between a request being made and a patient receiving care. To learn more about the Fast Prior Authorization Technology Highway (Fast PATH) initiative launched by AHIP and several health plans, consider attending Electronic Prior Authorization: The Fast PATH Towards Better Patient Care on August 25, 2021 at 2:00 PM – 3:00 PM ET.
Cutting Through Administrative Chaos by Focusing on Specific High-Value Use Cases
Surescripts Ashley Clark shared some actions that can be performed to cut through the chaos of everything that’s going on administratively at health plans and provider organizations. These included:
- Driving adoption and usage of a limited set of use cases by getting very specific about those use case
- How achieving success with a limited set of use cases can lead to bigger decisions across the board.
- Being very detailed about the information that is being shared back and forth so that it’s not seen as if irrelevant information were overlooked
Listen here for more from Surescripts Ashley Clark on cutting through administrative chaos
Plans and Providers Working Together to Avoid Duplicative Efforts
One participant whose organization is closely engaged with supporting provider organizations shared that when meeting with providers and health plans they talk regularly about “You both are doing the same things, you call them the same things. They’re a little bit different but why are you both doing Population Health Management?” He commented: “I don’t understand why people who are battling it out on engaging the patient are battling it out on collaboration at the level of administering clinical process.”
Who’s Best Positioned, Qualified, and Equipped to Own Specific Interoperability Use Cases
After discussing interoperability-focused use cases, roundtable participants shared their take on additional considerations regarding involvement and ownership. The following points were raised:
- Health plans are much better equipped to do population health management.
- Providers are much better equipped to deal with care requirements and patients in real-time.
- Everybody is investing in systems that are enormously expensive.
- Providers are spending a lot of money on tools that if they had better collaborative relationships with payers, they wouldn’t have to invest in.
Payers and providers each need to ask: What does practical interoperability mean for our business and how do we design our businesses?
Listen here for more from roundtable participants on interoperability-related use cases
Informing Care Decisions & Providing Insights to Either Side of the Network
As an individual who works directly with payers and who has colleagues working directly with providers, Tim Capstick shared that Surescripts tends to focus on informing care decisions, providing insights across the network to both sides of the network, and enhancing the prescribing process for providers.
Tim shared that on the payer side there is a lot of concern and issue around the consistency in which providers are utilizing enhanced prescribing services, what providers are getting out of prescription services enhanced by interoperability and the overall return on investment? And on the provider side: what is the quality of this information that’s being presented? Is data consistently being presented and can the data be trusted?
Listen here for more from Surescripts Tim Capstick on informing care decisions and increasing the adoption of interoperability use cases.
Additional Interoperability-related Topics of Discussion – Coming in Part 2
The first Focus Area Roundtable on Interoperability facilitated by Surescripts covered a lot of areas of interest to participants – way more than can be reasonably shared in a single post. In the second part of this two-part recap, information on the following will be shared:
- Trust, quality, and scarcity as a mechanism for increasing adoption of interoperability use cases
- The importance of balancing the amount of information payers share with providers
- Interoperability’s increasing importance and impact on value-based arrangements
- The importance of workflow
- An interesting comment about charging for access to healthcare data and how another participant responded
Come Learn More & Share Your Insight
Our second Focus Area Roundtable on Interoperability takes place on Tuesday, September 8th at 10:00 AM PT / 2:00 PM ET and will build upon the topics shared in the first roundtable. In addition, our Focus Area Partner Surescripts will share information on and respond to participant challenges, issues, and opportunities regarding interoperability collected in advance of the roundtable. Leaders of health plans, health systems, and provider organizations can request an invite here.
Special thanks to Ashley Clark and Tim Capstick of our sponsor Surescripts for sharing their unique insight in this roundtable. For information on any of the topics presented in this post, contact Tim Capstick or Ashley Clark.
To receive additional information on interoperability and other healthcare leader priorities on the 2021 HCEG Top 10+ list, subscribe to our newsletter and follow us on Twitter and LinkedIn.





[…] RELATED: How Health Plans Can Best Support Provider Organizations Address Barriers to Practical Interoperabil… […]
[…] RELATED: Health Plans as Primary Connection for Patients & Healthcare Consumers […]