Over the last 10+ years, nearly all health systems and healthcare providers have adopted some sort of electronic health record system (EHR). And since the start of the pandemic, these care providers have accelerated the use of telemedicine and remote patient monitoring tools to support their care management services. In addition, healthcare consumers are increasing their use of apps to manage their health, well-being, and related spending. These technology-based developments have enabled the collection of patient, clinical, and financial data in types and volumes never before possible; data that is essential to the operation of value-based payment programs.
Health Plans as ‘Keepers of the Data’ Need Advanced Care Management Capabilities
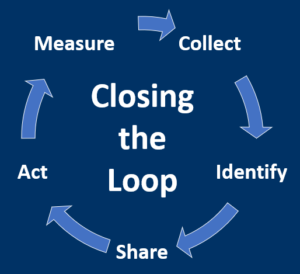
Moreover, recent regulations on data transparency, interoperability, and patients’ access to their data are strengthening health plans as a central repository of longitudinal aggregated data for plan members. By leveraging that data with technologies like artificial intelligence, machine learning, and robotic process automation, health plans are able to assist their provider networks with identifying, delivering, and closing the loop on the preventative, ‘whole-person’ and other population health management services critical to value-based programs.
RELATED: “Intelligent Care Management Technology: Driving Alignment Towards The Quadruple Aim” – Webinar, Thursday, October 7th, 2021 at 3:00 PM ET
Intelligent Care Management – Exceeding Typical Health Plan Capabilities
Intelligent Care Management Technologies (ICMT) go beyond the often disjointed utilization management, case management, and other clinically-focused services historically performed by health plans and provides an integrated, holistic approach to care.
Here are five reasons why health plans should be adopting Intelligent Care Management Technologies:
- Improves Patient Outcomes by Facilitating a Whole-Person Approach to Care
Being able to integrate, interpret, and efficiently utilize large data sets that span an individual’s entire health profile allows plans to help their provider network deliver insight and care at the right time and place. Potential life-threatening issues and medical complications can be caught sooner, enabling care providers to improve patient outcomes with fewer resources and at a lower cost.
- Extends Value of Provider Systems and Resources
Beyond not having a more complete patient profile, many care providers lack advanced analytics, guidelines, and tools that plans are better equipped to provide. The intelligent care management technologies shared by a health plan can positively impact provider practice patterns and improve overall care delivery to their patients and the plan’s members.
- Reduces Burden and Expense of Provider Network Partners
ICMT is integrated with existing provider and plan workflows with context, priority, and transparency to support faster and more informed care decisions by network physicians, nurses, and other care provider resources. Supporting clinicians helps to reduce the burden of increasing patient volumes and contributes to achieving the Quadruple Aim.
- Helps Address Social Determinants of Health and Leverages Community-Based Resources
ICMT helps tailor care based on social determinants of health, assessment tools, and guidelines to help identify, coordinate, and close the loop on services provided by network providers and local community-based organizations. Closing care gaps and assisting members and patients with obtaining medical and non-medical services from local organizations is an important part of value-based payment programs.
- Enables Health Plans to Assist Network Providers with Taking on More Risk
As care provider organizations and payers enter into more value-based care arrangements, it is critical for those organizations to strategically take on more risk and equitably share the cost of providing that care. Money spent on reactive care, avoidable hospital readmissions, and services performed in costly settings – among other things – are not only a waste of money but also burden increasingly scarce provider resources and negatively impact the patient experience. Intelligent Care Management Technologies allow plans to support their provider network by identifying, helping to coordinate and close the loop on proactive care across the care continuum.
RELATED: Intelligent Care Management Technologies: Key Considerations & Opportunities
Spreading Intelligence to Traditional Care Management
As the transition from fee-for-service to value-based payment programs accelerates and employers and consumers demand more their healthcare dollars, payers and providers must work with each other in more collaborative, intertwined ways. Utilizing intelligent care management technologies enables and supports the payer-provider collaboration essential to operating in today’s healthcare environment; and value-based arrangements in particular.
To learn more from healthcare leaders intimately involved with implementing and operating intelligent care management technologies, join us on Thursday, October 7th, 2021 at 3:00 PM ET for our live webinar “Intelligent Care Management Technology: Driving Alignment Towards The Quadruple Aim” presented by VirtualHealth.