We’ve analyzed the poll results from our webinar on Strategies to Improve Health Plan Margins on Public Insurance Exchanges. Get a firsthand look at the results. On March 29, 2016, we held a webinar in conjunction with AIS Health which gathered leading healthcare executives from health plans, health systems, and consulting firms. This presentation offered a valuable look into how qualified health plans (QHPs), and insurance carriers participating on health insurance exchanges, may minimize financial losses and achieve greater success. Offering a in-depth look of our reporting and analytic techniques for health plans doing business on ACA exchanges, the webinar polled participants on key topics relating to the current healthcare landscape. Here’s a sneak peak into the results.
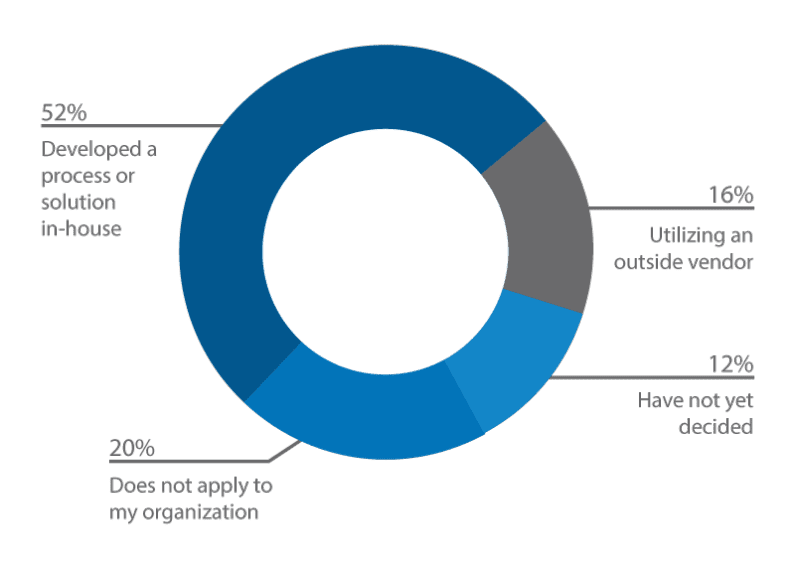
Poll #1: How is your organization handling its healthcare exchange analytics?
Voiced by the vast majority of respondents in our data set, organizations are handling their healthcare exchange analytics in-house via a developed process or solution (52%), followed by utilizing an outside vendor (16%), does not apply to my organization (20%), and lastly, have not decided (12%).
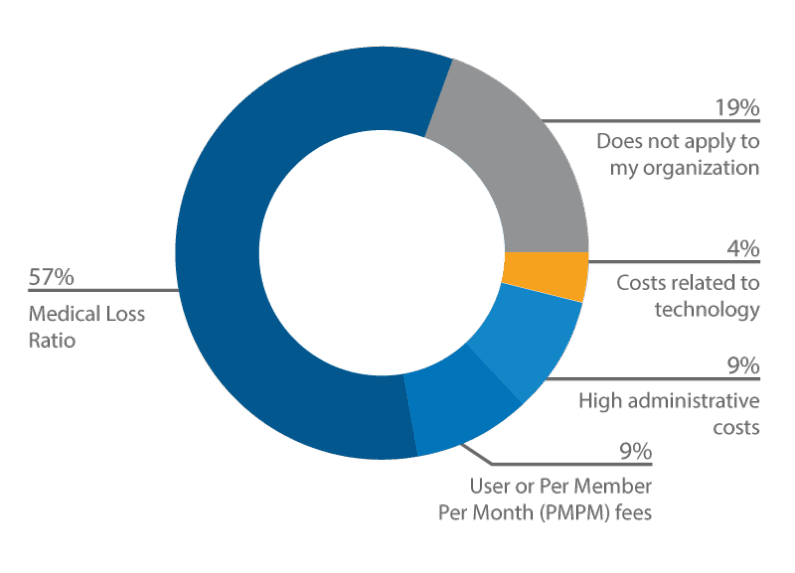
Poll #2: Currently, what is your biggest financial concern relating to your exchange business?
By a landslide, the majority of respondents have selected Medical Loss Raio as their biggest financial concern relating to their exchange business (57%), followed by does not apply to my organization (19%), User or Per Member Per Month (PMPM) fees (9%), high administrative costs (9%), and costs related to technology (4%).
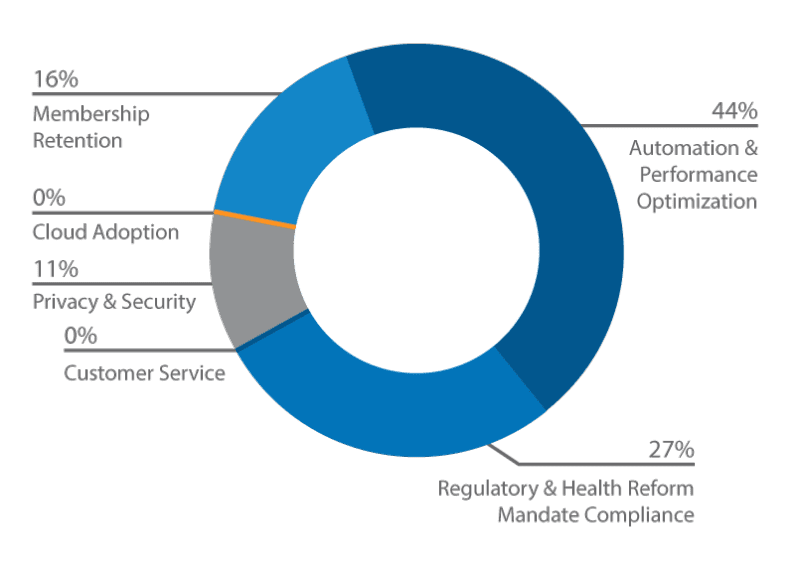
Poll #3: Which of the following do you anticipate as the next priority or opportunity for health payers?
Our poll indicates that among our participants, the next priority or opportunity for health payers will be automation & performance automation (44%), followed by regulatory & health reform mandate compliance (27%), membership retention (16%), and privacy & security (11%).
For more information on this webinar, contact us at[email protected]or access the webinar recording now.