Like other systemic changes needed to ‘fix healthcare’ in the United States that have been proposed, discussed, and tried in various forms and fashions over the last 20 years, the widespread, meaningful adoption of value-based payment programs seems to always be just a few years away. And now, the coronavirus pandemic has forced all healthcare stakeholders to re-think what is needed to truly transform the healthcare delivery system in the United States. In our first Focus Area Roundtable on Next-Generation Value-Based Payment Programs, participants discussed obstacles to value-based payment programs, selecting and measuring quality measures and outcomes, and topics related to engaging stakeholders – particularly payers and providers – collaboratively and in a proactive vs. reactive manner.
HCEG’s Executive Director Ferris Taylor and Eileen Lee, VP of Product – Connected Solutions, at Zelis Healthcare, helped facilitate discussion among roundtable participants: leaders from health plans, health systems, care provider organizations, and two consultants serving the healthcare industry. This post presents highlights of the roundtable. Individuals involved with transforming their provider reimbursement and payment systems are welcome to join our Focus Area Roundtables including the 2nd roundtable on Next-Generation Value-Based Payment Programs.
 Obstacles to Wider Adoption of Value-Based Payment Programs
Obstacles to Wider Adoption of Value-Based Payment Programs
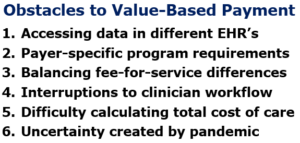
Ferris kicked off the roundtable by asking participants to share their thoughts on what obstacles are hampering the increased adoption of value-based care and payment programs.
Eileen Lee shared her perspective that many smaller, regional, commercial health plans simply don’t have the infrastructure or the resources to change the framework for how they process payments. She noted that with current infrastructures built around making fee-for-service payments (FFS) and high costs associated with implementing and administrating both FFS and value-based payment programs, the opportunity for these types of organizations to evolve is simply not available to them.
Expanding Provider Networks and Accessing Data in EHR’s
A chief technology officer of a health plan stated that their commercial plans still operate predominantly in a fee-for-service model and that they face two challenges in expanding their value-based payment footprint: developing their value-based provider networks and getting hospitals to participate and being able to connect into provider EHR systems to be able to send messages back and forth to support inpatient wellness and preventative health activities.
Eileen questioned whether engaging providers to participate in value-based programs was related to providers being unwilling to accept risk or whether they didn’t want the additional burden associated with collecting and reporting data.
One participant working with the front-line of care delivery shared that a big challenge for the front-line – from a value-based program’s perspective – is that collecting program metrics is ‘just another thing to do.’ She noted that if new data collection requirements can be better integrated into daily activities and workflow, value-based programs would be better accepted – particularly by physicians.
RELATED: Will Administrative Cost of Independent Dispute Resolution Force Providers to Join Networks?
Dealing with Different Requirements from Multiple Payers
In response to this comment on fitting into clinician workflow, Eileen reminded the roundtable that each payer has its own requirements and processes that clinicians must adhere to. The roundtable acknowledged the importance of recognizing and addressing payer-specific requirements, using standards and common definitions to the greatest extent possible, and selecting easily adaptable processes across multiple payers.
Capturing Meaningful Metrics as Part of Doing Business as Usual
One participant shared that, from his perspective, some Accountable Care Organization’s (ACO) are so concentrated on maximizing revenue by focusing on meeting quality measures and reporting end of year metrics, that innovations in care are not really welcomed. He noted that many metrics used for value-based programs should be captured and reported as a normal course of providing patient services – not just because they are required to receive specific payment program incentives.
The ability to incorporate data like laboratory values, medication lists, patient surveys, and other data that does not rely on inputs from clinicians or payers to support new payment models is one consideration noted in roundtable discussion.
Total Cost of Care Essential to Execute Value-Based Payment Programs
One participant associated with providing post-acute care in the home noted that the ability to accurately measure the total cost of care is key to being able to execute its value-based payment programs. She claimed that they don’t have access to all the data needed to be able to calculate the total cost of care.
Eileen asked if she thought that some of the transparency and coverage rule mandates will make calculating the total cost of care easier. The participant noted that they may if they were able to get eligibility data feeds to understand benefit coverage but obtaining that data is still up to the health plans to decide whether or not to share that data.
Measuring Quality, Outcomes, and Cost for Value-Based Payment Programs
Ferris asked the roundtable to share their thoughts on measuring quality, outcomes, and cost for value-based payment programs.
One participant noted their plan’s success with a value-based contract on heart failure using pharmaceuticals. He explained that what makes that agreement work is that it can be measured. They know when people take their medication whether it works for them or does not work for them based on claims data and information easily reported by the physician. And they have a very measurable outcome. He went on to say that costs savings can be measured using claims data.
Another participant, a manager of clinical integration at a regional, integrated healthcare provider/payer system, asked participants if it was possible for value-based care program outcomes to be measured with claims volume alone. And could a program be deemed ‘better’ due to the ability to measure its outcomes based on claims data alone without other patient artifacts in order to determine the quality of outcomes?
A health plan CIO stated that claims data alone is not enough in almost all cases and that clinical data is needed as well. Another person added that benchmarks are also needed to know how you’re performing relative to some baseline.
How the Pandemic has Impacted Value-Based Payment Programs
Eileen from Zelis questioned the group on how the pandemic has impacted value-based care. She noted that at the beginning of the pandemic, providers that were participating in value-based care and payment plans had a little bit less of an impact from the drop in service volumes. But now that patients have spent a year delaying care, Eileen wonders if providers are or will be seeing more negative outcomes even while they (physicians) are still providing the same historical level of care.
Providers Anticipating Increased Risk Due to Pandemic-Induced Delays to Care
Eileen went on to share observations on two trends emerging since the pandemic started in Q1 of 2020. She stated that there has been an increase in interest among providers in value-based care and value-based payments as a way to ward off the negative impacts of fee-for-service when patients stopped coming; noting providers see value-based payment programs as a leveling – a way to help manage their risk and keep their cash flow moving.
She added that she expects data to reveal the same trend about preventive care and about the severity of illness coming into ER’s that others are seeing. And wonders what that may mean for long-term outcomes and the measurement of those outcomes for purposes of value-based care payment. Eileen noted that it may be more difficult for physicians to get incentive payments and show high-quality metrics if their patients simply don’t participate in the care gap closing activities that they need to participate in order for there to be quality care outcomes. Listen here for pandemic’s impact on adoption of value-based payment programs [00:38:34 – 00:40:01]
Managing Patient Migration Outside the Network – Incentivizing Collaboration
One participant shared that supporting the ability of their network physicians to collaborate and communicate with other network physicians – and incentivizing them to do so – has had a large positive effect on both total cost of care point and outcomes relative to patient’s risk profile and chronic conditions: fewer ED visits and readmissions to inpatient care.
In line with comments made by Eileen Lee about the decrease in preventative services since the pandemic began, this participant noted that managing this so-called ‘migration outside the network’ has been hampered by the decrease in preventive care services utilized by many plan members and patients since the start of the pandemic in Q1 of 2020.
Other Considerations on Capturing Metrics and Improving Outcomes under Value-based Payment Programs
Participants shared insights and observations on other ways to capture metrics and improve outcomes under value-based payment programs – particularly as more and more services are moving from traditional acute care settings to community and home-based settings:
Delivering Care in the Home and Use of Remote Monitoring Technologies
One person noted seeing opportunities created for digital startups, especially remote patient monitoring startups where organizations can outsource some of the patient monitoring part and then receive great insights from these new companies only when it is needed. Listen here for more on new opportunities for supporting value-based payment programs [00:31:25 – 00:32:56]
Challenge in Accessing and Capturing Outcomes Data in the Home – Alleviated by OASIS Data?
Building on the idea of diagnosing, monitoring, and providing care in the home, Ferris asked one participant, a provider of post-acute services in the home, how they are capturing measures and outcomes data in the home care environment and whether that data is captured in an EHR.
The participant shared that, ideally, the delivery of home-based services would be integrated with EHRs but to do that they must obtain provider by provider approval to get access to providers’ EMR’s. She shared that another way they are looking at getting data is to try to get access to the Outcome and Assessment Information Set (OASIS) data because that is standard across all home health providers. She noted that using the OASIS data requires a technology solution to receive the data, integrate it into their technical architecture, and be able to manipulate and trend the data.
Impact of FHIR-Based Use Cases on Value-Based Payment Programs
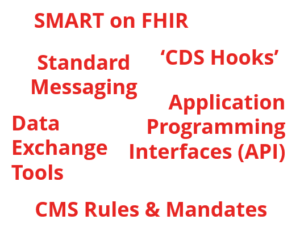
He also mentioned the use of new standard messaging and data exchange tools between payers and providers that utilize ‘CDS Hooks.’ Unfortunately, while the standards exist, leveraging them is still a one-on-one approach necessitating working with a FHIR vendor and integrating the back-and-forth integration.
While Ferris noted CMS’s Interoperability and Patient Access Final Rule now in effect as an example of a positive data exchange development between healthcare stakeholders, Eileen clarified that 67% of Americans are covered by self-funded or TPA plans that are not subject to the rule.
RELATED: Balancing Amount of Data Shared with Providers – Increasing Impact of Value-based Arrangements
Closing Thoughts on Next-Generation Value-Based Payment Programs
Ferris asked Eileen Lee of Zelis to wrap up the roundtable by offering a closing comment. Eileen shared that the adoption of value-based payment programs is one of those scenarios where the problem is easy to see and the solution seems even easier to decide but implementing it is complicated due to the diverse and diffuse environment of healthcare in the United States.
Listen here to Eileen Lee comment on the movement to Next-Generation Value-based Payment Programs [00:44:40 – 00:45:40]
Share Insight & Opinion on Value-Based Payment Programs and Join Our Next Roundtable
To assess payment-related challenges payers and providers are experiencing, identify gaps in the current payer-provider payment system, and help determine what’s holding back the adoption of new payer-provider payment solutions, the HealthCare Executive Group has created a mini-survey on Payer-Provider Payment Solutions. Healthcare stakeholders are urged to complete this three-minute survey. All survey respondents can receive survey results and be entered into a drawing for one of four $25 Amazon gift cards.
Join our next roundtable on Next-Generation Value-Based Payment Programs on Thursday, November 18, 2021, at 2:00 PM ET where additional insight, real-world experiences, and the latest developments on value-based payment programs will be discussed.
Join 7600+ other healthcare leaders and changemakers by subscribing to our newsletter and connecting with us on Twitter and LinkedIn.